Barrett's esophagus
| Barrett's esophagus | |
|---|---|
| Other names | Barrett's oesophagus, Allison-Johnstone anomaly, columnar epithelium lined lower oesophagus (CELLO) |
 | |
| Endoscopic image of Barrett's esophagus, which is the area of dark reddish-brown mucosa at the base of the esophagus. (Biopsies showed intestinal metaplasia.) | |
| Specialty | Gastroenterology General surgery |
| Symptoms | Nausea |
Barrett's esophagus is a condition in which there is an abnormal (metaplastic) change in the mucosal cells lining the lower portion of the esophagus, from stratified squamous epithelium to simple columnar epithelium with interspersed goblet cells that are normally present only in the small intestine and large intestine. This change is considered to be a premalignant condition because of its potential to further transition to esophageal adenocarcinoma, an often-deadly cancer.[1][2]
The main cause of Barrett's esophagus is thought to be an adaptation to chronic acid exposure from reflux esophagitis.[3] Barrett's esophagus is diagnosed by endoscopy: observing the characteristic appearance of this condition by direct inspection of the lower esophagus; followed by microscopic examination of tissue from the affected area obtained from biopsy. The cells of Barrett's esophagus are classified into four categories: nondysplastic, low-grade dysplasia, high-grade dysplasia, and frank carcinoma. High-grade dysplasia and early stages of adenocarcinoma may be treated by endoscopic resection or radiofrequency ablation.[4] Later stages of adenocarcinoma may be treated with surgical resection or palliation. Those with nondysplastic or low-grade dysplasia are managed by annual observation with endoscopy, or treatment with radiofrequency ablation. In high-grade dysplasia, the risk of developing cancer might be at 10% per patient-year or greater.[1]
The incidence of esophageal adenocarcinoma has increased substantially in the Western world in recent years.[1] The condition is found in 5–15% of patients who seek medical care for heartburn (gastroesophageal reflux disease, or GERD), although a large subgroup of patients with Barrett's esophagus are asymptomatic. The condition is named after surgeon Norman Barrett (1903–1979) even though the condition was originally described by Philip Rowland Allison in 1946.[5][6][7]
Signs and symptoms
[edit]The change from normal to premalignant cells in Barrett's esophagus typically does not cause specific symptoms. However, Barrett's esophagus is often associated with the following symptoms, primarily due to underlying gastroesophageal reflux disease (GERD):[8]
- frequent and longstanding heartburn
- trouble swallowing (dysphagia)
- vomiting blood (hematemesis)
- pain under the sternum where the esophagus meets the stomach
- pain when swallowing (odynophagia), which can lead to unintentional weight loss
The risk of developing Barrett's esophagus is increased by central obesity (vs. peripheral obesity).[9] The exact mechanism is unclear. The difference in distribution of fat among men (more central) and women (more peripheral) may explain the increased risk in males.[10]
Pathophysiology
[edit]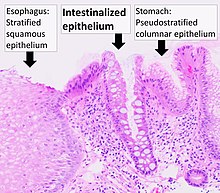
Barrett's esophagus occurs due to chronic inflammation. The principal cause of chronic inflammation is gastroesophageal reflux disease, GERD (UK: GORD). In this disease, acidic stomach, bile, and small intestine and pancreatic contents cause damage to the cells of the lower esophagus. In turn, this provokes an advantage for cells more resistant to these noxious stimuli in particular HOXA13-expressing stem cells that are characterised by distal (intestinal) characteristics and outcompete the normal squamous cells.[11]
This mechanism also explains the selection of HER2/neu (also called ERBB2) and the overexpressing (lineage-addicted) cancer cells during the process of carcinogenesis, and the efficacy of targeted therapy against the Her-2 receptor with trastuzumab (Herceptin) in the treatment of adenocarcinomas at the gastroesophageal junction.[citation needed]
Researchers are unable to predict who with heartburn will develop Barrett's esophagus. While no relationship exists between the severity of heartburn and the development of Barrett's esophagus, a relationship does exist between chronic heartburn and the development of Barrett's esophagus. Sometimes, people with Barrett's esophagus have no heartburn symptoms at all.[citation needed]
Some anecdotal evidence indicates those with the eating disorder bulimia are more likely to develop Barrett's esophagus because bulimia can cause severe acid reflux, and because purging also floods the esophagus with acid. However, a link between bulimia and Barrett's esophagus remains unproven.[12][13]
During episodes of reflux, bile acids enter the esophagus, and this may be an important factor in carcinogenesis.[14] Individuals with GERD and BE are exposed to high concentrations of deoxycholic acid that has cytotoxic effects and can cause DNA damage.[14][15]
Diagnosis
[edit]


Both macroscopic (from endoscopy) and microscopic positive findings are required to make a diagnosis. Barrett's esophagus is marked by the presence of columnar epithelia in the lower esophagus, replacing the normal squamous cell epithelium—an example of metaplasia. The secretory columnar epithelium may be more able to withstand the erosive action of the gastric secretions; however, this metaplasia confers an increased risk of adenocarcinoma.[16]
Screening
[edit]
Screening endoscopy is recommended among males over the age of 60 who have reflux symptoms that are of long duration and not controllable with treatment.[17] Among those not expected to live more than five years screening is not recommended.[17]
The Seattle protocol is used commonly in endoscopy to obtain endoscopic biopsies for screening, taken every 1 to 2 cm from the gastroesophageal junction.[citation needed]
Since the COVID-19 pandemic In Scotland, the local NHS started using a swallowable sponge (Cytosponge) in hospitals to collect cell samples for diagnosis.[18] Preliminary studies have shown this diagnostic test to be a useful tool for screening people with heartburn symptoms and improved diagnosis.[19][20]
Other emerging technologies for screening and diagnosis include optical coherence tomography (OCT), which can generate high-resolution images of the esophagus with moderate sensitivity and specificity for detecting Barrett's esophagus, though it may not yet be accurate enough to replace standard biopsies.[21]
Intestinal metaplasia
[edit]The presence of goblet cells, called intestinal metaplasia, is necessary to make a diagnosis of Barrett's esophagus. This frequently occurs in the presence of other metaplastic columnar cells, but only the presence of goblet cells is diagnostic. The metaplasia is grossly visible through a gastroscope, but biopsy specimens must be examined under a microscope to determine whether cells are gastric or colonic in nature. Colonic metaplasia is usually identified by finding goblet cells in the epithelium and is necessary for the true diagnosis.[22][citation needed]
Many histologic mimics of Barrett's esophagus are known (i.e. goblet cells occurring in the transitional epithelium of normal esophageal submucosal gland ducts, "pseudogoblet cells" in which abundant foveolar [gastric] type mucin simulates the acid mucin true goblet cells). Assessment of relationship to submucosal glands and transitional-type epithelium with examination of multiple levels through the tissue may allow the pathologist to reliably distinguish between goblet cells of submucosal gland ducts and true Barrett's esophagus (specialized columnar metaplasia). The histochemical stain Alcian blue pH 2.5 is also frequently used to distinguish true intestinal-type mucins from their histologic mimics. Recently, immunohistochemical analysis with antibodies to CDX-2 (specific for mid and hindgut intestinal derivation) has also been used to identify true intestinal-type metaplastic cells. The protein AGR2 is elevated in Barrett's esophagus[23] and can be used as a biomarker for distinguishing Barrett epithelium from normal esophageal epithelium.[24]
The presence of intestinal metaplasia in Barrett's esophagus represents a marker for the progression of metaplasia towards dysplasia and eventually adenocarcinoma. This factor combined with two different immunohistochemical expression of p53, Her2 and p16 leads to two different genetic pathways that likely progress to dysplasia in Barrett's esophagus.[25] Also intestinal metaplastic cells can be positive for CK 7+/CK20-.[26]
Epithelial dysplasia
[edit]After the initial diagnosis of Barrett's esophagus is rendered, affected persons undergo annual surveillance to detect changes that indicate higher risk to progression to cancer: development of epithelial dysplasia (or "intraepithelial neoplasia").[27] Among all metaplastic lesions, around 8% were associated with dysplasia. particularly a recent study demonstrated that dysplastic lesions were located mainly in the posterior wall of the esophagus.[28]
Considerable variability is seen in assessment for dysplasia among pathologists. Recently, gastroenterology and GI pathology societies have recommended that any diagnosis of high-grade dysplasia in Barrett be confirmed by at least two fellowship-trained GI pathologists prior to definitive treatment for patients.[16] For more accuracy and reproducibility, it is also recommended to follow international classification systems, such as the "Vienna classification" of gastrointestinal epithelial neoplasia (2000).[29]
Management
[edit]Many people with Barrett's esophagus do not have dysplasia. Medical societies recommend that if a patient has Barrett's esophagus, and if the past two endoscopy and biopsy examinations have confirmed the absence of dysplasia, then the patient should not have another endoscopy within three years.[30][31][32]
Endoscopic surveillance of people with Barrett's esophagus is often recommended, although little direct evidence supports this practice.[1] Treatment options for high-grade dysplasia include surgical removal of the esophagus (esophagectomy) or endoscopic treatments such as endoscopic mucosal resection or ablation (destruction).[1]
The risk of malignancy is highest in the United States in Caucasian men over fifty years of age with more than five years of symptoms. Current recommendations include routine endoscopy and biopsy (looking for dysplastic changes). Although in the past physicians have taken a watchful waiting approach, newly published research supports consideration of intervention for Barrett's esophagus. Balloon-based radiofrequency ablation, invented by Ganz, Stern, and Zelickson in 1999, is a new treatment modality for the treatment of Barrett's esophagus and dysplasia and has been the subject of numerous published clinical trials.[33][34][35][36] The findings demonstrate radiofrequency ablation is at least 90% effective to completely clear Barrett's esophagus and dysplasia, with durability of up to five years and a favorable safety profile.[33][34][35][36]
Anti-reflux surgery has not been proven to prevent esophageal cancer. However, the indication[who?] is that proton pump inhibitors are effective in limiting the progression of esophageal cancer[citation needed]. Laser treatment is used in severe dysplasia, while overt malignancy may require surgery, radiation therapy, or systemic chemotherapy. A recent five-year random-controlled trial has shown that photodynamic therapy using photofrin is statistically more effective in eliminating dysplastic growth areas than sole use of a proton pump inhibitor.[37]
There is presently no reliable way to determine which patients with Barrett's esophagus will go on to develop esophageal cancer, although a recent study found the detection of three different genetic abnormalities was associated with as much as a 79% chance of developing cancer in six years.[38]
Endoscopic mucosal resection has also been evaluated as a management technique.[39] Additionally an operation known as a Nissen fundoplication can reduce the reflux of acid from the stomach into the esophagus.[40]
In a variety of studies, nonsteroidal anti-inflammatory drugs (NSAIDS) such as low-dose aspirin (75–300 mg/day) have shown evidence of preventing esophageal cancer in people with Barrett's esophagus.[41][42][43][44]
Prognosis
[edit]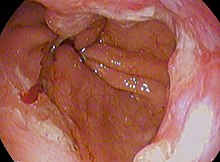
adenocarcinoma (poor; signet-ringcell)
Barrett's esophagus is a pre-malignant condition, not a cancerous one.[citation needed]
A small subset of patients with Barrett's esophagus will eventually develop malignant esophagogastric junctional adenocarcinoma, which has a mortality rate of over 85%.[45]
The risk of developing esophageal adenocarcinoma increases based on how severe the Barrett's esophagus has become.[46] Longer length of the Barrett's esophagus region is also associated with increased risk of developing cancer.[46][47]
Progression and severity of Barrett's esophagus is measured by amount of dysplasia the cells show. Dysplasia is scored on a five-tier system:[47]
- negative for dysplasia (non-dysplastic Barrett's esophagus or NDBE)
- indefinite for dysplasia (IND)
- low-grade dysplasia (LGD)
- high-grade dysplasia (HGD)
- carcinoma
A 2016 study found that the rate of progression to esophageal adenocarcinoma in Barrett's esophagus patients with no dysplasia, low-grade dysplasia, and high-grade dysplasia are around 0.6%, 13.4%, and 25%, respectively.[48]
However, for low-grade dysplasia, the true yearly rate of progression to cancer remains difficult to estimate, as results are highly variable from study to study, from 13.4% down to 0.84%.[46] This is partly due to each study having a different mix of intermediate disease states being combined under the umbrella diagnosis of LGD.[47] There is also some concern that risk may be slightly overestimated in the literature due to publication bias.[49][50]
Epidemiology
[edit]The incidence in the United States among Caucasian men is eight times the rate among Caucasian women and five times greater than African American men. Overall, the male to female ratio of Barrett's esophagus is 10:1.[51] Several studies have estimated the prevalence of Barrett's esophagus in the general population to be 1.3% to 1.6% in two European populations (Italian[52] and Swedish[53]), and 3.6% in a Korean population.[54]
History
[edit]The condition is named after Australian thoracic surgeon Norman Barrett (1903–1979), who in 1950 argued that "ulcers are found below the squamocolumnar junction ... represent gastric ulcers within 'a pouch of stomach ... drawn up by scar tissue into the mediastinum' ... representing an example of a 'congenital short esophagus'".[55][56] In contrast, Philip Rowland Allison and Alan Johnstone argued that the condition related to the "esophagus lined with gastric mucous membrane and not intra-thoracic stomach as Barrett mistakenly believed."[57][6] Philip Allison, cardiothoracic surgeon and Chair of Surgery at the University of Oxford, suggested "calling the chronic peptic ulcer crater of the esophagus a 'Barrett's ulcer'", but added this name did not imply agreement with "Barrett's description of an esophagus lined with gastric mucous membrane as stomach."[57][6] Bani-Hani KE and Bani-Hani KR argue that the terminology and definition of Barrett's esophagus is surrounded by extraordinary confusion unlike most other medical conditions and that "[t]he use of the eponym 'Barrett's' to describe [the condition] is not justified from a historical point of view".[6] Bani-Hani KE and Bani-Hani KR investigated the historical aspects of the condition and found they could establish "how little Norman Barrett had contributed to the core concept of this condition in comparison to the contributions of other investigators, particularly the contribution of Philip Allison".[6]
A further association was made with adenocarcinoma in 1975.[58]
References
[edit]- ^ a b c d e Shaheen NJ, Richter JE (March 2009). "Barrett's oesophagus". Lancet. 373 (9666): 850–61. doi:10.1016/S0140-6736(09)60487-6. PMID 19269522. S2CID 13141959.
- ^ Koppert LB, Wijnhoven BP, van Dekken H, Tilanus HW, Dinjens WN (December 2005). "The molecular biology of esophageal adenocarcinoma". Journal of Surgical Oncology. 92 (3): 169–90. doi:10.1002/jso.20359. PMID 16299787. S2CID 42893278.
- ^ Stein HJ, Siewert JR (1993). "Barrett's esophagus: pathogenesis, epidemiology, functional abnormalities, malignant degeneration, and surgical management". Dysphagia. 8 (3): 276–88. doi:10.1007/BF01354551. PMID 8359051. S2CID 6715044.
- ^ Shaheen, Nicholas J.; Falk, Gary W.; Iyer, Prasad G.; Gerson, Lauren B.; American College of Gastroenterology (January 2016). "ACG Clinical Guideline: Diagnosis and Management of Barrett's Esophagus". The American Journal of Gastroenterology. 111 (1): 30–50, quiz 51. doi:10.1038/ajg.2015.322. ISSN 1572-0241. PMC 10245082. PMID 26526079. S2CID 2274838.
- ^ Allison PR (March 1948). "Peptic ulcer of the oesophagus". Thorax. 3 (1): 20–42. doi:10.1136/thx.3.1.20. PMC 1018255. PMID 18904843.
- ^ a b c d e Bani-Hani KE, Bani-Hani BK (May 2008). "Columnar-lined esophagus: time to drop the eponym of "Barrett": Historical review". Journal of Gastroenterology and Hepatology. 23 (5): 707–15. doi:10.1111/j.1440-1746.2008.05386.x. PMID 18410605. S2CID 21531132.
- ^ Katz-Summercorn, Annalise C.; Frankell, Alexander M.; Fitzgerald, Rebecca C. (2016). "Chapter 4: Genetics and Biomarkers in Barrett's Esophagus and Esophageal Adenocarcinoma". In Pleskow, Douglas K.; Erim, Tolga (eds.). Barrett's Esophagus - Emerging Evidence for Improved Clinical Practice. pp. 37–60. doi:10.1016/B978-0-12-802511-6.00004-1. ISBN 9780128025116.
- ^ "Barrett's Esophagus". Johns Hopkins Medicine. Retrieved 5 October 2024.
- ^ Edelstein ZR, Farrow DC, Bronner MP, Rosen SN, Vaughan TL (August 2007). "Central adiposity and risk of Barrett's esophagus". Gastroenterology. 133 (2): 403–11. doi:10.1053/j.gastro.2007.05.026. PMID 17681161.
- ^ Reid BJ, Li X, Galipeau PC, Vaughan TL (February 2010). "Barrett's oesophagus and oesophageal adenocarcinoma: time for a new synthesis". Nature Reviews. Cancer. 10 (2): 87–101. doi:10.1038/nrc2773. PMC 2879265. PMID 20094044.
- ^ Janmaat VT, Nesteruk K, Spaander MC, Verhaar AP, Yu B, Silva RA, Phillips WA, Magierowski M, van de Winkel A, Stadler HS, Sandoval-Guzmán T, van der Laan LJ, Kuipers EJ, Smits R, Bruno MJ, Fuhler GM, Clemons NJ, Peppelenbosch MP (Jun 2021). "HOXA13 in etiology and oncogenic potential of Barrett's esophagus". Nature Communications. 12 (1): 3354. Bibcode:2021NatCo..12.3354J. doi:10.1038/s41467-021-23641-8. PMC 8184780. PMID 34099670.
- ^ Navab, Farhad; Avunduk, Canan; Gang, David; Frankel, Kenneth (1996). "Bulimia nervosa complicated by Barrett's esophagus and esophageal cancer". Gastrointestinal Endoscopy. 44 (4): 492–494. doi:10.1016/S0016-5107(96)70110-4. PMID 8905379. Retrieved 28 July 2018.
- ^ "Bulimia and cancer - what you need to know - Bulimia Help". Bulimiahelp.org. Archived from the original on 23 July 2018. Retrieved 28 July 2018.
- ^ a b Jürgens, S.; Meyer, F.; Spechler, S. J.; Souza, R. (September 2012). "The role of bile acids in the neoplastic progression of Barrett's esophagus - a short representative overview". Zeitschrift für Gastroenterologie. 50 (9): 1028–1034. doi:10.1055/s-0032-1312922. PMID 22965634. S2CID 1099567.
- ^ Bernstein, H.; Bernstein, C.; Payne, C. M.; Dvorakova, K.; Garewal, H. (January 2005). "Bile acids as carcinogens in human gastrointestinal cancers". Mutation Research. 589 (1): 47–65. doi:10.1016/j.mrrev.2004.08.001. PMID 15652226.
- ^ a b Fléjou JF (March 2005). "Barrett's oesophagus: from metaplasia to dysplasia and cancer". Gut. 54 (Suppl 1): i6–12. doi:10.1136/gut.2004.041525. PMC 1867794. PMID 15711008.
- ^ a b Bennett C, Moayyedi P, Corley DA, DeCaestecker J, Falck-Ytter Y, Falk G, et al. (May 2015). "BOB CAT: A Large-Scale Review and Delphi Consensus for Management of Barrett's Esophagus With No Dysplasia, Indefinite for, or Low-Grade Dysplasia". The American Journal of Gastroenterology. 110 (5): 662–82, quiz 683. doi:10.1038/ajg.2015.55. PMC 4436697. PMID 25869390.
- ^ "Cytosponge". www.nhsinform.scot. Retrieved 2022-04-05.
- ^ "An innovative swallowable sponge detects Barrett's oesophagus in people with heartburn, study shows". NIHR Evidence (Plain English summary). 2021-02-16. doi:10.3310/alert_44006. S2CID 242399505.
- ^ Fitzgerald, Rebecca C; di Pietro, Massimiliano; O'Donovan, Maria; Maroni, Roberta; Muldrew, Beth; Debiram-Beecham, Irene; Gehrung, Marcel; Offman, Judith; Tripathi, Monika; Smith, Samuel G; Aigret, Benoit (1 August 2020). "Cytosponge-trefoil factor 3 versus usual care to identify Barrett's oesophagus in a primary care setting: a multicentre, pragmatic, randomised controlled trial". The Lancet. 396 (10247): 333–344. doi:10.1016/S0140-6736(20)31099-0. PMC 7408501. PMID 32738955.
- ^ Kohli, D. R.; Schubert, M. L.; Zfass, A. M.; Shah, T. U. (November 2017). "Performance characteristics of optical coherence tomography in assessment of Barrett's esophagus and esophageal cancer: systematic review". Diseases of the Esophagus. 30 (11): 1–8. doi:10.1093/dote/dox049.
- ^ "Barrett's Esophagus". The Lecturio Medical Concept Library. Retrieved 3 July 2021.
- ^ Pohler E, Craig AL, Cotton J, Lawrie L, Dillon JF, Ross P, et al. (June 2004). "The Barrett's antigen anterior gradient-2 silences the p53 transcriptional response to DNA damage". Molecular & Cellular Proteomics. 3 (6): 534–47. doi:10.1074/mcp.M300089-MCP200. PMID 14967811.
- ^ Murray E, McKenna EO, Burch LR, Dillon J, Langridge-Smith P, Kolch W, et al. (December 2007). "Microarray-formatted clinical biomarker assay development using peptide aptamers to anterior gradient-2". Biochemistry. 46 (48): 13742–51. doi:10.1021/bi7008739. PMID 17994709.
- ^ Salemme M, Villanacci V, Cengia G, Cestari R, Missale G, Bassotti G (February 2016). "Intestinal metaplasia in Barrett's oesophagus: An essential factor to predict the risk of dysplasia and cancer development". Digestive and Liver Disease. 48 (2): 144–7. doi:10.1016/j.dld.2015.10.021. PMID 26614646.
- ^ Çoban Ş, Örmeci N, Savaş B, Ekiz F, Ensari A, Kuzu I, Palabıyıkoğlu M (2013). "Evaluation of Barrett's esophagus with CK7, CK20, p53, Ki67, and COX2 expressions using chromoendoscopical examination". Diseases of the Esophagus. 26 (2): 189–96. doi:10.1111/j.1442-2050.2012.01352.x. PMID 22591041.
- ^ Odze RD (October 2006). "Diagnosis and grading of dysplasia in Barrett's oesophagus". Journal of Clinical Pathology. 59 (10): 1029–38. doi:10.1136/jcp.2005.035337. PMC 1861756. PMID 17021130.
- ^ Bibbò, S; Ianiro, G; Ricci, R; Arciuolo, D; Petruzziello, L; Spada, C; Larghi, A; Riccioni, ME; Gasbarrini, A; Costamagna, G; Cammarota, G (Sep 2016). "Barrett's oesophagus and associated dysplasia are not equally distributed within the esophageal circumference". Dig Liver Dis. 48 (9): 1043–7. doi:10.1016/j.dld.2016.06.020. PMID 27436487.
- ^ Schlemper RJ, Riddell RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, et al. (August 2000). "The Vienna classification of gastrointestinal epithelial neoplasia". Gut. 47 (2): 251–5. doi:10.1136/gut.47.2.251. PMC 1728018. PMID 10896917.
- ^ American Gastroenterological Association, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American Gastroenterological Association, archived from the original (PDF) on August 9, 2012, retrieved August 17, 2012
- ^ Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ (March 2011). "American Gastroenterological Association medical position statement on the management of Barrett's esophagus". Gastroenterology. 140 (3): 1084–91. doi:10.1053/j.gastro.2011.01.030. PMID 21376940.
- ^ Wang KK, Sampliner RE (March 2008). "Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus". The American Journal of Gastroenterology. 103 (3): 788–97. doi:10.1111/j.1572-0241.2008.01835.x. PMID 18341497. S2CID 8443847.
- ^ a b Fleischer DE, Overholt BF, Sharma VK, Reymunde A, Kimmey MB, Chuttani R, et al. (October 2010). "Endoscopic radiofrequency ablation for Barrett's esophagus: 5-year outcomes from a prospective multicenter trial". Endoscopy. 42 (10): 781–9. doi:10.1055/s-0030-1255779. PMID 20857372. S2CID 24224546.
- ^ a b Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, et al. (May 2009). "Radiofrequency ablation in Barrett's esophagus with dysplasia". The New England Journal of Medicine. 360 (22): 2277–88. doi:10.1056/NEJMoa0808145. PMID 19474425.
- ^ a b Shaheen NJ, Overholt BF, Sampliner RE, Wolfsen HC, Wang KK, Fleischer DE, et al. (August 2011). "Durability of radiofrequency ablation in Barrett's esophagus with dysplasia". Gastroenterology. 141 (2): 460–8. doi:10.1053/j.gastro.2011.04.061. PMC 3152658. PMID 21679712.
- ^ a b van Vilsteren FG, Pouw RE, Seewald S, Alvarez Herrero L, Sondermeijer CM, Visser M, Ten Kate FJ, Yu Kim Teng KC, Soehendra N, Rösch T, Weusten BL, Bergman JJ (June 2011). "Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett's oesophagus with high-grade dysplasia or early cancer: a multicentre randomised trial". Gut. 60 (6): 765–73. doi:10.1136/gut.2010.229310. PMID 21209124. S2CID 38316532.
- ^ Overholt BF, Wang KK, Burdick JS, Lightdale CJ, Kimmey M, Nava HR, et al. (September 2007). "Five-year efficacy and safety of photodynamic therapy with Photofrin in Barrett's high-grade dysplasia". Gastrointestinal Endoscopy. 66 (3): 460–8. doi:10.1016/j.gie.2006.12.037. PMID 17643436.
- ^ Galipeau PC, Li X, Blount PL, Maley CC, Sanchez CA, Odze RD, et al. (February 2007). "NSAIDs modulate CDKN2A, TP53, and DNA content risk for progression to esophageal adenocarcinoma". PLOS Medicine. 4 (2): e67. doi:10.1371/journal.pmed.0040067. PMC 1808095. PMID 17326708.
- ^ Reshamwala PA, Darwin PE (September 2006). "Endoscopic management of early gastric cancer". Current Opinion in Gastroenterology. 22 (5): 541–5. doi:10.1097/01.mog.0000239870.04457.80. PMID 16891887. S2CID 12959801.
- ^ Abbas AE, Deschamps C, Cassivi SD, Allen MS, Nichols FC, Miller DL, et al. (February 2004). "Barrett's esophagus: the role of laparoscopic fundoplication". The Annals of Thoracic Surgery. 77 (2): 393–6. doi:10.1016/S0003-4975(03)01352-3. PMID 14759403.
- ^ Corley DA, Kerlikowske K, Verma R, Buffler P (January 2003). "Protective association of aspirin/NSAIDs and esophageal cancer: a systematic review and meta-analysis". Gastroenterology. 124 (1): 47–56. doi:10.1053/gast.2003.50008. PMID 12512029.
- ^ Vaughan TL, Dong LM, Blount PL, Ayub K, Odze RD, Sanchez CA, Rabinovitch PS, Reid BJ (December 2005). "Non-steroidal anti-inflammatory drugs and risk of neoplastic progression in Barrett's oesophagus: a prospective study". The Lancet. Oncology. 6 (12): 945–52. doi:10.1016/S1470-2045(05)70431-9. PMID 16321762.
- ^ García Rodríguez, Luis A.; Soriano-Gabarró, Montse; Vora, Pareen; Cea Soriano, Lucía (7 May 2020). "Low-dose aspirin and risk of gastric and oesophageal cancer: A population-based study in the United Kingdom using The Health Improvement Network". International Journal of Cancer. 147 (9): 2394–2404. doi:10.1002/ijc.33022. ISSN 0020-7136. PMC 7540378. PMID 32329063.
- ^ Schieszer, John (29 September 2019). "Study Shows Association Between Low-Dose Aspirin Use and Risk for Gastric and Esophageal Cancers". Oncology Nurse Advisor.
- ^ Holmes RS, Vaughan TL (January 2007). "Epidemiology and pathogenesis of esophageal cancer". Seminars in Radiation Oncology. 17 (1): 2–9. doi:10.1016/j.semradonc.2006.09.003. PMID 17185192.
- ^ a b c Li S, Hoefnagel S, Krishnadath KK (November 2023). "Molecular Biology and Clinical Management of Esophageal Adenocarcinoma". Cancers. 15 (22): 5410. doi:10.3390/cancers15225410. PMC 10670638. PMID 38001670.
- ^ a b c Stawinski PM, Dziadkowiec KN, Kuo LA, Echavarria J, Saligram S (January 2023). "Barrett's Esophagus: An Updated Review". Diagnostics. 13 (2): 321. doi:10.3390/diagnostics13020321. PMC 9858189. PMID 36673131.
- ^ Greyson EM, Bornschein J, Fitzgerald RC (July 2016). "Genetic progression of Barrett's oesophagus to oesophageal adenocarcinoma". British Journal of Cancer. 115 (4): 403–410. doi:10.1038/bjc.2016.219. PMC 4985359. PMID 27441494.
- ^ Shaheen, Nicholas J.; et al. (August 2000). "Is there publication bias in the reporting of cancer risk in Barrett's esophagus?". Gastroenterology. 119 (2): 333–338. doi:10.1053/gast.2000.9302.
- ^ Spechler, Stuart Jon (August 2000). "Barrett's esophagus: An overrated cancer risk factor". Gastroenterology. 119 (2): 587–589. doi:10.1053/gast.2000.9849. PMID 10930393.
- ^ Zajac, P; Holbrook, A; Super, ME; Vogt, M (March–April 2013). "An overview: Current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia". Osteopathic Family Physician. 5 (2): 79–85. doi:10.1016/j.osfp.2012.10.005.
- ^ Zagari RM, Fuccio L, Wallander MA, Johansson S, Fiocca R, Casanova S, et al. (October 2008). "Gastro-oesophageal reflux symptoms, oesophagitis and Barrett's oesophagus in the general population: the Loiano-Monghidoro study". Gut. 57 (10): 1354–9. doi:10.1136/gut.2007.145177. PMID 18424568. S2CID 206947077.
- ^ Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, et al. (December 2005). "Prevalence of Barrett's esophagus in the general population: an endoscopic study". Gastroenterology. 129 (6): 1825–31. doi:10.1053/j.gastro.2005.08.053. PMID 16344051.
- ^ Kim JY, Kim YS, Jung MK, Park JJ, Kang DH, Kim JS, et al. (April 2005). "Prevalence of Barrett's esophagus in Korea". Journal of Gastroenterology and Hepatology. 20 (4): 633–6. doi:10.1111/j.1440-1746.2005.03749.x. PMID 15836715. S2CID 46543142.
- ^ Barrett NR (October 1950). "Chronic peptic ulcer of the oesophagus and 'oesophagitis'". The British Journal of Surgery. 38 (150): 175–82. doi:10.1002/bjs.18003815005. PMID 14791960. S2CID 72315839.
- ^ DeMeester SR, DeMeester TR (March 2000). "Columnar mucosa and intestinal metaplasia of the esophagus: fifty years of controversy". Annals of Surgery. 231 (3): 303–21. doi:10.1097/00000658-200003000-00003. PMC 1421001. PMID 10714623.
- ^ a b Allison PR, Johnstone AS (June 1953). "The oesophagus lined with gastric mucous membrane". Thorax. 8 (2): 87–101. doi:10.1136/thx.8.2.87. PMC 1019247. PMID 13077502.
- ^ Naef AP, Savary M, Ozzello L (November 1975). "Columnar-lined lower esophagus: an acquired lesion with malignant predisposition. Report on 140 cases of Barrett's esophagus with 12 adenocarcinomas". The Journal of Thoracic and Cardiovascular Surgery. 70 (5): 826–35. doi:10.1016/s0022-5223(19)39666-7. PMID 1186274.
